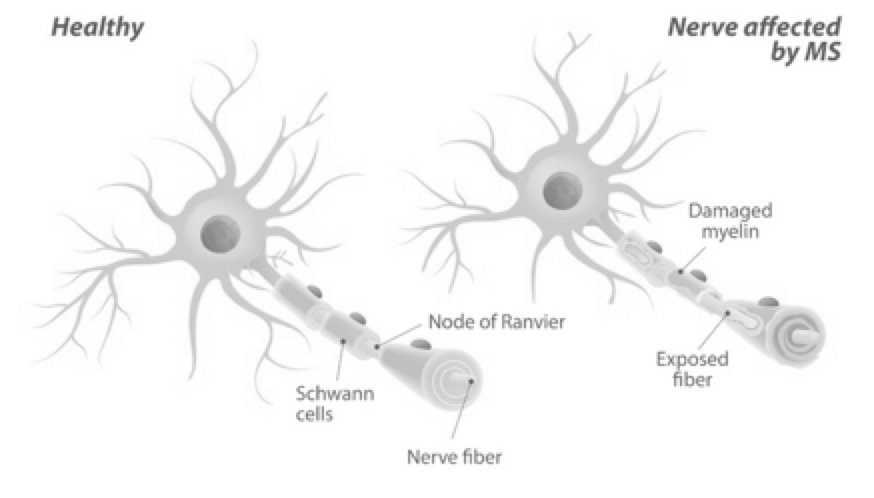
Multiple sclerosis (MS) is an inflammatory, demyelinating auto-immune disease of the central nervous system (CNS) affecting ~1 million patients in the United States and a total ~3 million patients globally. Activated immune cells invade the CNS causing inflammation, neurodegeneration (destruction of the myelin sheaths protecting nerve fibers) and tissue damage (lesions/ plaques). Damage to myelin “short circuits” communication between the brain, spinal cord and other areas of the body, severely impairing such neurological functions as mobility, vision and thinking. Over time, the nerves themselves can become permanently damaged.
Most people are diagnosed with MS between the ages of 20 and 50, although it can develop in individuals as young as 2 and as old as 75 with most patients developing the disease between the ages of 20 and 40.
The underlying cause of MS is yet unknown; the current understanding is that MS is not a single disease but rather a spectrum, and there is scientific debate ongoing whether MS is to be considered an auto-immune disease or not. Course and prognosis depend on diverse factors (subtype, sex, age, symptoms, degree of disability) with a life expectancy of ~30 years from onset corresponding to an approximate loss of 5-10 years lifetime. While ~40% of patients reach age of 70, two-thirds of deaths are directly related to MS.
MS drugs have generated US$ 24 billion sales in 2018 globally. However, the vast majority of approved treatments has label indications for the relapsing-remitting form with the aim to manage the inflammatory component of the disease. While managing inflammation in MS is a “crowded space”, countering neural degeneration, i.e. destruction of the myelin sheaths surrounding neurons, is a large unmet need where approved disease-modifying therapies do not work well. Most approved agents have limited penetration of the blood brain barrier and hence, while they can dampen down the immune system and inflammation in the periphery, do not stop the ongoing disease in the brain. Also, treatments do not support reconstituting demyelinated nerves. A disease modifying treatment with neuro-reparative and neuroprotective properties is urgently needed.
Our research suggests sPIF may cross the blood-brain-barrier in MS patients, and in an interrelated manner promote re-myelination and reduce neuronal inflammation and degeneration, in the brain, the spine and peripheral nerves.